
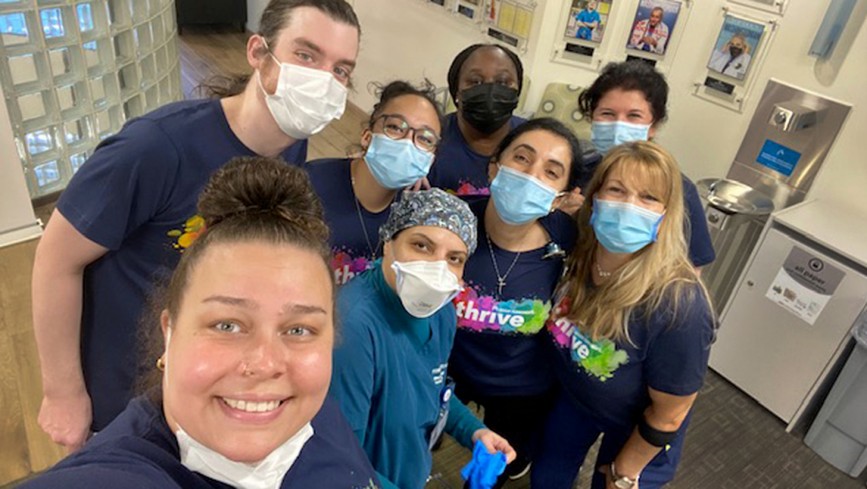
Members of the Mid-Valley Addiction Medicine team collect patient demographic information to customize care options.
Teams collect patient demographic information
Jenna Li and Autum Tomlin serve in different specialties at opposite ends of the country. Yet each plays a central part in efforts to harness patient data to improve care and eliminate health disparities at Kaiser Permanente.
Li is a chemical dependency counselor with the Mid-Valley Addiction Medicine team in Salem, Oregon. Members of her unit-based team, represented by Alliance-affiliated unions, make standard practice of asking patients about their sexual orientation, gender identity and preferred pronouns.
Tomlin is an urgent care technician at Reston Medical Center in Virginia. She and her team – represented by Alliance- and Coalition-affiliated unions – collect information about patients’ race, ethnicity, and preferred language. She has seen, first-hand, the power of speaking to patients in words they can understand.
“Usually, you can see the patient is at ease and feels a sense of relief that they are able to communicate in their preferred language,” says Tomlin, the team’s labor co-lead and a member of OPEIU Local 2, part of the Coalition of Kaiser Permanente Unions.
Like others across the organization, the Level 5 unit-based teams are seeking to address disparities in health and access to quality care that persist across a range of dimensions – including race, language, gender, and sexual orientation. By asking patients about their backgrounds in a safe, respectful, and compassionate way, the teams are changing how they deliver care and service to members – and relate to one another.
“The effort is minimal, and the effectiveness can be really high when we help a patient feel seen and understood,” says Li, labor co-lead for the Mid-Valley team and a member of OFNHP Local 5017, part of the Alliance of Health Care Unions.
Making members feel welcome
To better understand patients’ health risks and needs, the Mid-Valley team began asking members about their sexual orientation and gender information. They asked the questions during the intake assessment and entered patients’ responses into their electronic health records, making important background information available to all KP providers.
The practice is already changing how the Northwest team delivers care to LGBTQ+ patients.
For instance, Mid-Valley is referring more members to a weekly group therapy session for LGBTQ+ patients to discuss their unique challenges. Misunderstandings about sexual orientation or gender identity are among the obstacles such patients face in accessing effective care. They also are at elevated risk from health threats including alcohol and substance abuse.
Recently, the team hustled to track down a teen-ager in crisis who had fled their clinic’s waiting room. Knowing the teen identified as nonbinary, staff members convinced them to return after expressing sensitivity to their fears and addressing them with their preferred pronouns.
Gestures to support these patients are especially important because they come to treatment reeling from the “double whammy” of stigmatization for their addiction struggles and LGTBQ+ identity.
“We can do a lot to make a member feel welcome by using language they are open to hearing,” says Carri McCrary, Mid-Valley clinical services manager and the team’s management co-lead.
Members of the urgent care team in Reston got to know each other better through their performance improvement project.
Learning about each other
In Reston, Virginia, urgent care team members developed better working relationships as a result of asking patients about their preferred language.
Urgent Care is often the first point of contact for new Kaiser Permanente members – and a vital opportunity for staff to collect patient demographic information.
Knowing a patient’s primary language is crucial for delivering optimal care and treatment. Language barriers are associated with worse health outcomes, lower patient satisfaction, and increased use of some services, including more emergency room visits and longer clinic visits.
Kaiser Permanente patients who need language assistance can request interpreter services and have materials translated into their language, or in alternative formats, at no cost.
In helping patients communicate, team members discovered that several colleagues spoke multiple languages and could serve as interpreters. The process was revealing.
“It helped us learn a lot about each other,” says Tomlin. “It brought us together and has been a really good thing.”
